In Vitro Fertilization
(IVF)
In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.

In Vitro Fertilization
(IVF)
In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.
During IVF, mature eggs are collected from ovaries and fertilized by sperm in a laboratory. Then the fertilized egg (embryo) or eggs (embryos) are transferred to a uterus. One full cycle of IVF takes about three weeks. Sometimes these steps are split into different parts and the process can take longer.
IVF is the most effective form of assisted reproductive technology. The procedure can be done using your own eggs and your partner’s sperm.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. If more than one embryo is transferred to your uterus, IVF can result in a pregnancy with more than one fetus (multiple pregnancies).
Your doctor can help you understand how IVF works, the potential risks, and whether this method of treating infertility is right for you.
Why it's done



In vitro fertilization (IVF) is a treatment for infertility or genetic problems. If IVF is performed to treat infertility, you and your partner might be able to try less-invasive treatment options before attempting IVF, including fertility drugs to increase production of eggs or intrauterine insemination — a procedure in which sperm are placed directly in your uterus near the time of ovulation.
Sometimes, IVF is offered as a primary treatment for infertility in women over age 40. IVF can also be done if you have certain health conditions. For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.
- Endometriosis. Endometriosis occurs when the uterine tissue implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are benign tumors in the wall of the uterus and are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
- Previous tubal sterilization or removal. If you’ve had tubal ligation — a type of sterilization in which your fallopian tubes are cut or blocked to permanently prevent pregnancy — and want to conceive, IVF may be an alternative to tubal ligation reversal.
- Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg. If semen abnormalities are found, your partner might need to see a specialist to determine if there are correctable problems or underlying health concerns.
- Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, you may be candidates for preimplantation genetic testing — a procedure that involves IVF. After the eggs are harvested and fertilized, they’re screened for certain genetic problems, although not all genetic problems can be found. Embryos that don’t contain identified problems can be transferred to the uterus.
Fertility preservation for cancer or other health conditions. If you’re about to start cancer treatment — such as radiation or chemotherapy — that could harm your fertility, IVF for fertility preservation may be an option. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
Women who don’t have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy (gestational carrier). In this case, the woman’s eggs are fertilized with sperm, but the resulting embryos are placed in the gestational carrier’s uterus.
Risks
Risks of IVF include:
- Multiple births. IVF increases the risk of multiple births if more than one embryo is transferred to your uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does.
- Premature delivery and low birth weight. Research suggests that IVF slightly increases the risk that the baby will be born early or with a low birth weight.
Ovarian hyperstimulation syndrome. Use of injectable fertility drugs, such as human chorionic gonadotropin (HCG), to induce ovulation can cause ovarian hyperstimulation syndrome, in which your ovaries become swollen and painful.
Symptoms typically last a week and include mild abdominal pain, bloating, nausea, vomiting and diarrhea. If you become pregnant, however, your symptoms might last several weeks. Rarely, it’s possible to develop a more severe form of ovarian hyperstimulation syndrome that can also cause rapid weight gain and shortness of breath.
- Miscarriage. The rate of miscarriage for women who conceive using IVF with fresh embryos is similar to that of women who conceive naturally — about 15% to 25% — but the rate increases with maternal age.
- Egg-retrieval procedure complications. Use of an aspirating needle to collect eggs could possibly cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also associated with sedation and general anesthesia, if used.
- Ectopic pregnancy. About 2% to 5% of women who use IVF will have an ectopic pregnancy — when the fertilized egg implants outside the uterus, usually in a fallopian tube. The fertilized egg can’t survive outside the uterus, and there’s no way to continue the pregnancy.
- Birth defects. The age of the mother is the primary risk factor in the development of birth defects, no matter how the child is conceived. More research is needed to determine whether babies conceived using IVF might be at increased risk of certain birth defects.
- Cancer. Although some early studies suggested there may be a link between certain medications used to stimulate egg growth and the development of a specific type of ovarian tumor, more-recent studies do not support these findings. There does not appear to be a significantly increased risk of breast, endometrial, cervical or ovarian cancer after IVF.
- Stress. Use of IVF can be financially, physically and emotionally draining. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.

How you prepare
Before beginning a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screenings, including:
- Ovarian reserve testing. To determine the quantity and quality of your eggs, your doctor might test the concentration of follicle-stimulating hormone (FSH), estradiol (estrogen), and anti-mullerian hormone in your blood during the first few days of your menstrual cycle. Test results often used together with an ultrasound of your ovaries, can help predict how your ovaries will respond to fertility medication.
- Semen analysis. If not done as part of your initial fertility evaluation, your doctor will conduct a semen analysis shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for infectious diseases, including HIV.
- Practice (mock) embryo transfer. Your doctor might conduct a mock embryo transfer to determine the depth of your uterine cavity and the technique most likely to successfully place the embryos into your uterus.
- Uterine exam. Your doctor will examine the inside lining of the uterus before you start IVF. This might involve a sonohysterography — in which fluid is injected through the cervix into your uterus — and an ultrasound to create images of your uterine cavity. Or it might include a hysteroscopy — in which a thin, flexible, lighted telescope (hysteroscope) is inserted through your vagina and cervix into your uterus.
Before beginning a cycle of IVF, consider important questions, including:
How many embryos will be transferred? The number of embryos transferred is typically based on age and the number of eggs retrieved. Since the rate of implantation is lower for older women, more embryos are usually transferred — except for women using donor eggs or genetically tested embryos.
Most doctors follow specific guidelines to prevent higher-order multiple pregnancies — triplets or more — and in some countries, legislation limits the number of embryos that can be transferred. Make sure you and your doctor agree on the number of embryos that will be transferred before the transfer procedure.
What will you do with any extra embryos? Extra embryos can be frozen and stored for future use for several years. Not all embryos will survive the freezing and thawing process, although most will.
Cryopreservation can make future cycles of IVF less expensive and less invasive. Or, you might be able to donate unused frozen embryos to another couple or a research facility. You might also choose to discard unused embryos.
- How will you handle multiple pregnancies? If more than one embryo is transferred to your uterus, IVF can result in multiple pregnancies — which poses health risks for you and your babies. In some cases, the fetal reduction can be used to help a woman deliver fewer babies with lower health risks. Pursuing fetal reduction, however, is a major decision with ethical, emotional, and psychological consequences.
- Have you considered the potential complications associated with using donor eggs, sperm or embryos, or a gestational carrier? A trained counselor with expertise in donor issues can help you understand the concerns, such as the legal rights of the donor. You may also need an attorney to file court papers to help you become legal parents of an implanted embryo.
What you can expect
IVF involves several steps — ovarian stimulation, egg retrieval, sperm retrieval, fertilization, and embryo transfer. One cycle of IVF can take about two to three weeks, and more than one cycle may be required.
Ovulation Induction
If you’re using your own eggs during IVF, at the start of a cycle you’ll begin treatment with synthetic hormones to stimulate your ovaries to produce multiple eggs — rather than the single egg that normally develops each month. Multiple eggs are needed because some eggs won’t fertilize or develop normally after fertilization.
You may need several different medications, such as:
- Medications for ovarian stimulation. To stimulate your ovaries, you might receive an injectable medication containing a follicle-stimulating hormone (FSH), a luteinizing hormone (LH), or a combination of both. These medications stimulate more than one egg to develop at a time.
- Medications for oocyte maturation. When the follicles are ready for egg retrieval — generally after eight to 14 days — you will take human chorionic gonadotropin (HCG) or other medications to help the eggs mature.
- Medications to prevent premature ovulation. These medications prevent your body from releasing the developing eggs too soon.
- Medications to prepare the lining of your uterus. On the day of egg retrieval or at the time of embryo transfer, your doctor might recommend that you begin taking progesterone supplements to make the lining of your uterus more receptive to implantation.
Your doctor will work with you to determine which medications to use and when to use them.
Typically, you’ll need one to two weeks of ovarian stimulation before your eggs are ready for retrieval. To determine when the eggs are ready for collection, your doctor will likely perform:
- Vaginal ultrasound, an imaging exam of your ovaries to monitor the development of follicles — fluid-filled ovarian sacs where eggs mature
- Blood tests, to measure your response to ovarian stimulation medications — estrogen levels typically increase as follicles develop, and progesterone levels remain low until after ovulation
Sometimes IVF cycles need to be canceled before egg retrieval for one of these reasons:
- Inadequate number of follicles developing
- Premature ovulation
- Too many follicles developing, creating a risk of ovarian hyperstimulation syndrome
- Other medical issues
If your cycle is canceled, your doctor might recommend changing medications or their doses to promote a better response during future IVF cycles. Or you may be advised that you need an egg donor.
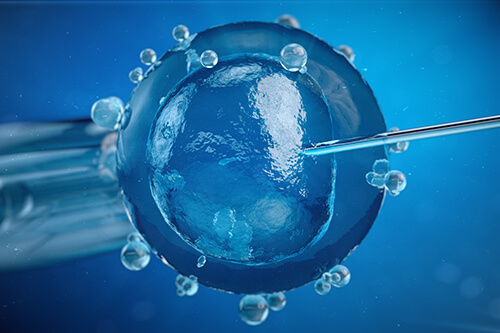
Egg Retrieval
Egg retrieval can be done in your doctor’s office or a clinic 34 to 36 hours after the final injection and before ovulation.
- During egg retrieval, you’ll be sedated and given pain medication.
- Transvaginal ultrasound aspiration is the usual retrieval method. An ultrasound probe is inserted into your vagina to identify follicles. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to retrieve the eggs.
- If your ovaries aren’t accessible through transvaginal ultrasound, an abdominal ultrasound may be used to guide the needle.
- The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
- After egg retrieval, you may experience cramping and feelings of fullness or pressure.
- Mature eggs are placed in a nutritive liquid (culture medium) and incubated. Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
Sperm Retrieval
If you’re using your partner’s sperm, he’ll provide a semen sample at your doctor’s office or a clinic through masturbation the morning of egg retrieval. Other methods, such as testicular aspiration — the use of a needle or surgical procedure to extract sperm directly from the testicle — are sometimes required. Donor sperm also can be used. Sperm are separated from the semen fluid in the lab.

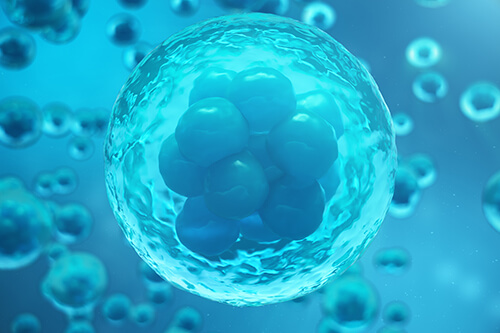
Fertilization
Fertilization can be attempted using two common methods:
- Conventional insemination. During conventional insemination, healthy sperm and mature eggs are mixed and incubated overnight.
- Intracytoplasmic sperm injection (ICSI). In ICSI, a single healthy sperm is injected directly into each mature egg. ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
In certain situations, your doctor may recommend other procedures before embryo transfer.
- Assisted hatching. About five to six days after fertilization, an embryo “hatches” from its surrounding membrane (zona pellucida), allowing it to implant into the lining of the uterus. If you’re an older woman, or if you have had multiple failed IVF attempts, your doctor might recommend assisted hatching — a technique in which a hole is made in the zona pellucida just before transfer to help the embryo hatch and implant. Assisted hatching is also useful for eggs or embryos that have been previously frozen as the process can harden the zona pellucida.
- Preimplantation genetic testing. Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don’t contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can’t eliminate the risk. Prenatal testing may still be recommended.
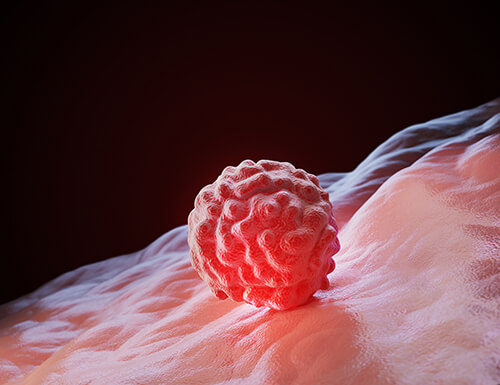
Embryo Transfer
Embryo transfer is done at your doctor’s office or a clinic and usually takes place two to five days after egg retrieval.
- You might be given a mild sedative. The procedure is usually painless, although you might experience mild cramping.
- The doctor will insert a long, thin, flexible tube called a catheter into your vagina, through your cervix, and into your uterus.
- A syringe containing one or more embryos suspended in a small amount of fluid is attached to the end of the catheter.
- Using the syringe, the doctor places the embryo or embryos into your uterus.
If successful, an embryo will implant in the lining of your uterus about six to 10 days after egg retrieval.

After the Procedure
After the embryo transfer, you can resume normal daily activities. However, your ovaries may still be enlarged. Consider avoiding vigorous activity, which could cause discomfort.
Typical side effects include:
- Passing a small amount of clear or bloody fluid shortly after the procedure — due to the swabbing of the cervix before the embryo transfer
- Breast tenderness due to high estrogen levels
- Mild bloating
- Mild cramping
- Constipation
If you develop moderate or severe pain after the embryo transfer, contact your doctor. He or she will evaluate you for complications such as infection, twisting of an ovary (ovarian torsion), and severe ovarian hyperstimulation syndrome.
Results
About 12 days to two weeks after egg retrieval, your doctor will test a sample of your blood to detect whether you’re pregnant.
- If you’re pregnant, your doctor will refer you to an obstetrician or other pregnancy specialist for prenatal care.
- If you’re not pregnant, you’ll stop taking progesterone and likely get your period within a week. If you don’t get your period or you have unusual bleeding, contact your doctor. If you’re interested in attempting another cycle of in vitro fertilization (IVF), your doctor might suggest steps you can take to improve your chances of getting pregnant through IVF.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF. Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success.
- Embryo status. Transfer of embryos that are more developed is associated with higher pregnancy rates compared with less developed embryos (day two or three). However, not all embryos survive the development process. Talk with your doctor or another care provider about your specific situation.
- Reproductive history. Women who’ve previously given birth are more likely to be able to get pregnant using IVF than are women who’ve never given birth. Success rates are lower for women who’ve previously used IVF multiple times but didn’t get pregnant.
- Cause of infertility. Having a normal supply of eggs increases your chances of being able to get pregnant using IVF. Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility.
- Lifestyle factors. Women who smoke typically have fewer eggs retrieved during IVF and may miscarry more often. Smoking can lower a woman’s chance of success using IVF by 50%. Obesity can decrease your chances of getting pregnant and having a baby. Use of alcohol, recreational drugs, excessive caffeine, and certain medications also can be harmful.
Talk with your doctor about any factors that apply to you and how they may affect your chances of a successful pregnancy.