Obesity
Obesity is a complex disease involving an excessive amount of body fat. Obesity isn’t just a cosmetic concern. It is a medical problem that increases your risk of other diseases and health problems, such as heart disease, diabetes, high blood pressure and certain cancers.
Obesity is diagnosed when your body mass index (BMI) is 30 or higher.

Obesity
Obesity is a complex disease involving an excessive amount of body fat. Obesity isn’t just a cosmetic concern. It is a medical problem that increases your risk of other diseases and health problems, such as heart disease, diabetes, high blood pressure and certain cancers.
Obesity is diagnosed when your body mass index (BMI) is 30 or higher.
Complications
People with obesity are more likely to develop a number of potentially serious health problems, including:

Heart disease and strokes
Obesity makes you more likely to have high blood pressure and abnormal cholesterol levels, which are risk factors for heart disease and strokes.

Type 2 diabetes
Obesity can affect the way your body uses insulin to control blood sugar levels. This raises your risk of insulin resistance and diabetes.
Certain cancers
Obesity may increase your risk of cancer of the uterus, cervix, endometrium, ovary, breast, colon, rectum, esophagus, liver, gallbladder, pancreas, kidney and prostate.
Digestive problems
Obesity increases the likelihood that you'll develop heartburn, gallbladder disease and liver problems.
Gynecological and sexual problems
Obesity may cause infertility and irregular periods in women. Obesity also can cause erectile dysfunction in men.
Sleep apnea
People with obesity are more likely to have sleep apnea, a potentially serious disorder in which breathing repeatedly stops and starts during sleep.
Quality of life
Obesity can diminish your overall quality of life. You may not be able to do things you used to do, such as participating in enjoyable activities. You may avoid public places. People with obesity may even encounter discrimination.
Other weight-related issues that may affect your quality of life include:
- Depression
- Disability
- Sexual problems
- Shame and guilt
- Social isolation
- Lower work achievement
Prevention from obesity
Whether you’re at risk of obesity, currently overweight or at a healthy weight, you can take steps to prevent unhealthy weight gain and related health problems. Not surprisingly, the steps to prevent weight gain are the same as the steps to lose weight: daily exercise, a healthy diet, and a long-term commitment to watch what you eat and drink.
Exercise regularly
You need to get 150 to 300 minutes of moderate-intensity activity a week to prevent weight gain. Moderately intense physical activities include fast walking and swimming.
Follow a healthy-eating plan
Focus on low-calorie, nutrient-dense foods, such as fruits, vegetables and whole grains. Avoid saturated fat and limit sweets and alcohol. Eat three regular meals a day with limited snacking. You can still enjoy small amounts of high-fat, high-calorie foods as an infrequent treat. Just be sure to choose foods that promote a healthy weight and good health most of the time.
Know and avoid the food traps that cause you to eat
Identify situations that trigger out-of-control eating. Try keeping a journal and write down what you eat, how much you eat, when you eat, how you’re feeling and how hungry you are. After a while, you should see patterns emerge. You can plan ahead and develop strategies for handling these types of situations and stay in control of your eating behaviors.
Monitor your weight regularly
People who weigh themselves at least once a week are more successful in keeping off excess pounds. Monitoring your weight can tell you whether your efforts are working and can help you detect small weight gains before they become big problems.
Be consistent
Sticking to your healthy-weight plan during the week, on the weekends, and amidst vacation and holidays as much as possible increases your chances of long-term success.
Treatment
The goal of obesity treatment is to reach and stay at a healthy weight. This improves your overall health and lowers your risk of developing complications related to obesity. You may need to work with a team of health professionals — including a dietitian, behavioral counselor or an obesity specialist — to help you understand and make changes in your eating and activity habits.
Dietary changes
Reducing calories and practicing healthier eating habits are vital to overcoming obesity. Although you may lose weight quickly at first, steady weight loss over the long term is considered the safest way to lose weight and the best way to keep it off permanently.
The key to weight loss is reducing how many calories you take in. The first step is to review your typical eating and drinking habits to see how many calories you normally consume and where you can cut back. You and your doctor can decide how many calories you need to take in each day to lose weight, but a typical amount is 1,200 to 1,500 calories for women and 1,500 to 1,800 for men.
Certain diets limit the amount of a particular food group, such as high-carbohydrate or full-fat foods. Ask your doctor which diet plans have been found effective and which might be helpful for you. Drinking sugar-sweetened beverages is a sure way to consume more calories than you intended, and limiting these drinks or eliminating them altogether is a good place to start cutting calories.
Exercise and activity
Increased physical activity or exercise is an essential part of obesity treatment. Most people who are able to maintain their weight loss for more than a year get regular exercise, even simply walking.
People with obesity need to get at least 150 minutes a week of moderate-intensity physical activity to prevent further weight gain or to maintain the loss of a modest amount of weight. To achieve more-significant weight loss, you may need to exercise 300 minutes or more a week.
Prescription weight-loss medication
Losing weight requires a healthy diet and regular exercise. But in certain situations, prescription weight-loss medication may help.
Your doctor may recommend weight-loss medication if other diet and exercise programs haven’t worked and you meet one of these criteria:
- Your body mass index (BMI) is 30 or greater
- Your BMI is greater than 27, and you also have medical complications of obesity, such as diabetes, high blood pressure or sleep apnea
Anti-obesity medications approved by the Food and Drug Administration (FDA) include:
- Orlistat (Alli, Xenical)
- Lorcaserin (Belviq)
- Phentermine and topiramate (Qsymia)
- Bupropion and naltrexone (Contrave)
- Liraglutide (Saxenda, Victoza)
You’ll need close medical monitoring while taking a prescription weight-loss medication. Also, keep in mind that a weight-loss medication may not work for everyone, and the effects may wane over time. When you stop taking a weight-loss medication, you may regain much or all of the weight you lost.
Endoscopic procedures for weight loss
These types of procedures don’t require any incisions in your skin. After you receive anesthesia, flexible tubes and tools are inserted through your mouth and down your throat into your stomach.
There are several different types of endoscopic procedures used for weight loss. One procedure involves placing stitches in your stomach to reduce its size and the amount of food you can comfortably consume. In another endoscopic procedure, doctors insert a small balloon into your stomach. The balloon is filled with water to reduce the amount of space available in your stomach. This helps you feel fuller faster.
These procedures are usually approved for people with BMIs of 30 or above when diet and exercise alone have not been successful. The expected weight loss varies among procedures from 5% to 20% of total body weight loss.
Weight-loss surgery
In some people, weight-loss surgery, also called bariatric surgery, is an option. Weight-loss surgery limits the amount of food you’re able to comfortably eat or decreases the absorption of food and calories, or it does both. While weight-loss surgery offers the best chance of losing the most weight, it can pose serious risks.
Weight-loss surgery for obesity may be considered if you have tried other methods to lose weight that haven’t worked and:
- You have extreme obesity (BMI of 40 or higher)
- Your BMI is 35 to 39.9, and you also have a serious weight-related health problem, such as diabetes or high blood pressure
- You’re committed to making the lifestyle changes that are necessary for surgery to work
Weight-loss surgery helps some people lose as much as 35% or more of their excess body weight. But weight-loss surgery isn’t a miracle obesity cure.
It doesn’t guarantee that you’ll lose all of your excess weight or that you’ll keep it off long term. Weight-loss success after surgery depends on your commitment to making lifelong changes in your eating and exercise habits.

Common weight-loss surgeries include:
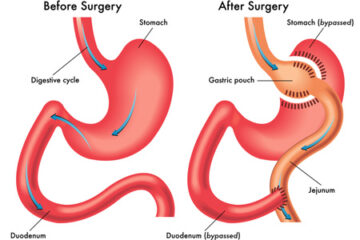
Gastric bypass surgery
In gastric bypass (Roux-en-Y gastric bypass), the surgeon creates a small pouch at the top of your stomach. The small intestine is then cut a short distance below the main stomach and connected to the new pouch. Food and liquid flow directly from the pouch into this part of the intestine, bypassing most of your stomach.
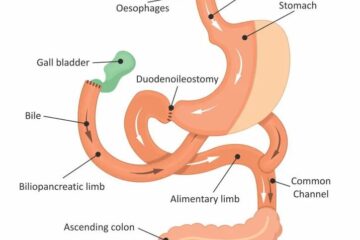
Biliopancreatic diversion with duodenal switch
This procedure begins with the surgeon removing a large part of the stomach. The surgeon leaves the valve that releases food to the small intestine and the first part of the small intestine (duodenum). Then the surgeon closes off the middle section of the intestine and attaches the last part directly to the duodenum. The separated section of the intestine is reattached to the end of the intestine to allow bile and digestive juices to flow into this part of the intestine.
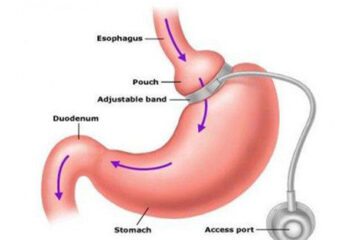
Adjustable gastric banding
In this procedure, your stomach is separated into two pouches with an inflatable band. Pulling the band tight, like a belt, the surgeon creates a tiny channel between the two pouches. The band keeps the opening from expanding and is generally designed to stay in place permanently.
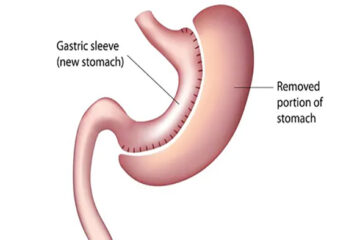
Sleeve Gastrectomy
In this procedure, part of the stomach is removed, creating a smaller reservoir for food. It’s a less complicated surgery than gastric bypass or biliopancreatic diversion with duodenal switch.
Sleeve gastrectomy is done to help you lose excess weight and reduce your risk of potentially life-threatening weight-related health problems, including:
- Gastroesophageal reflux disease
- Heart disease
- High blood pressure
- High cholesterol
- Obstructive sleep apnea
- Type 2 diabetes
- Stroke
- Infertility
Sleeve gastrectomy is typically done only after you’ve tried to lose weight by improving your diet and exercise habits.
In general, sleeve gastrectomy surgery could be an option for you if:
- Your body mass index (BMI) is 40 or higher (extreme obesity).
- Your BMI is 35 to 39.9 (obesity), and you have a serious weight-related health problem, such as type 2 diabetes, high blood pressure or severe sleep apnea. In some cases, you may qualify for certain types of weight-loss surgery if your BMI is 30 to 34 and you have serious weight-related health problems.
You must also be willing to make permanent changes to lead a healthier lifestyle. You may be required to participate in long-term follow-up plans that include monitoring your nutrition, your lifestyle and behavior, and your medical conditions.